Polycystic Ovarian Syndrome (PCOS)
INTRODUCTION:
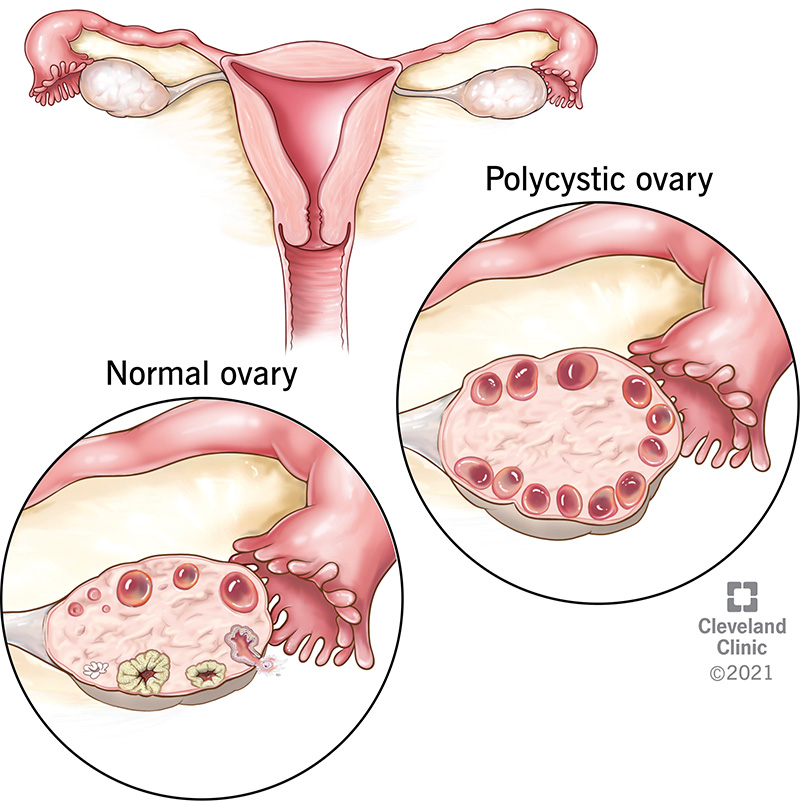
Polycystic ovary syndrome (PCOS), a heterogeneous, complex genetic trait of unclear, and likely multiple, etiology, is an important cause of ovulatory and menstrual irregularity, subfertility and infertility, clinically evident hyperandrogenism, and metabolic dysfunction in women. When fully expressed, the manifestations include ovulatory dysfunction, androgen excess, and polycystic ovaries. It is recognized as one of the most common endocrine/metabolic disorders of women. This syndrome was first described by Stein and Leventhal in 1935 [1], although the presence of sclerocystic ovaries had been recognized for at least 90 years prior to their report.
The definition, epidemiology, and pathogenesis (including genetics) of PCOS will be reviewed here. The clinical manifestations, diagnosis, and treatment of PCOS are discussed separately.
PHENOTYPES OF PCOS:
In general, four different phenotypes of PCOS are considered and should be referred to when making the diagnosis of PCOS:
●Phenotype A (also known as "full PCOS" or "classic PCOS") includes biochemical or clinical hyperandrogenism, oligoovulation, and polycystic ovarian morphology
●Phenotype B (also known as "classic PCOS") includes hyperandrogenism and oligoanovulation
●Phenotype C (also known as "ovulatory PCOS") includes hyperandrogenism and polycystic ovarian morphology
●Phenotype D (also known as "non-hyperandrogenic PCOS") includes oligoanovulation and polycystic ovarian morphology
PATHOGENESIS:
Gonadotropin secretion and action:
Altered LH action appears to be involved in the pathogenesis of PCOS, as illustrated by the following:
●PCOS patients often have higher serum LH concentrations and increased LH pulse frequency and amplitude than matched controls. However, serum LH tends to be lower in obese women with PCOS compared with their lean counterparts.
●LH action at the ovarian level may be enhanced in PCOS as the LH receptor is overexpressed in thecal and granulosa cells from polycystic ovaries.
●Genetic variants of the LH beta-subunit and loci near FSHR, LHCGR, and FSHB in GWAS have been reported in patients with PCOS.
The increased LH to follicle-stimulating hormone (FSH) ratio further enhances hypersecretion of androgens in the theca cells in the ovarian follicles. The increase in follicular androgens impairs follicular development and reduces the normal inhibition of gonadotropin-releasing hormone (GnRH) pulse frequency by progesterone, further promoting the development of the PCOS phenotype. In addition, there is evidence of resistance to the effects of FSH at the follicular levels in the ovaries of PCOS women, possibly in part secondary to excess local anti-müllerian hormone (AMH) production Increased LH pulses and enhanced daytime LH pulse secretion are also observed early during puberty in girls with hyperandrogenism [65], suggesting that abnormalities in the pulsatile release of GnRH might underlie the development of PCOS, at least in some patients.
Dysfunction in ovarian folliculogenesis:
In PCOS, the selection of a dominant follicle is abnormal, a consequence of insufficient FSH stimulation and local inhibition of FSH action, possibly due to excess local AMH and other intra-ovarian factors that modulate follicular recruitment and growth. Increased pituitary secretion of FSH alone, for example, through the administration of antiestrogens such as clomiphene citrate or aromatase inhibitors (letrozole), will often result in the resumption of normal follicular growth and ovulation in PCOS.
Insulin secretion and action:
It was first observed that patients with PCOS were hyperinsulinemic in response to an oral glucose tolerance test [69]. It is now known that insulin resistance, and the development of compensatory hyperinsulinemia, is a frequent finding in PCOS. The insulin resistance and hyperinsulinemia of PCOS patients that underlies many of the features of this disorder is highlighted by the finding that the administration of insulin-sensitizing agents, principally metformin, thiazolidinediones, and d-chiro-inositol, has been found to improve these features in many patients.
Obesity and energy regulation:
The presence of obesity worsens insulin resistance, the degree of hyperinsulinemia, the severity of ovulatory and menstrual dysfunction, and pregnancy outcome in PCOS and is associated with an increasing prevalence of metabolic syndrome, glucose intolerance, cardiovascular risk factors, and sleep apnea.
Androgen biosynthesis and action:
Hyperandrogenism is a central feature for most forms (phenotypes A through C) of PCOS. The androgens are secreted primarily by the ovaries and secondarily by the adrenals. Although hyperinsulinism is associated with hyperandrogenism in PCOS, insulin resistance alone is not sufficient for the development of PCOS, suggesting that an underlying (genetic) predisposition to hyperandrogenism must also be present.
Environmental factors:
The most clearly defined environmental factor likely affecting the development of PCOS is diet and its association with obesity. Nonetheless, despite wide variations in the prevalence of obesity and type of diet, the prevalence of PCOS appears to be relatively uniform across the globe.
Clinical Manifestations Of PCOS:
The symptoms of PCOS may include:
•Missed periods, irregular periods, or very light periods
•Ovaries that are large or have many cysts
•Excess body hair, including the chest, stomach, and back (hirsutism)
•Weight gain, especially around the belly (abdomen)
•Acne or oily skin
•Male-pattern baldness or thinning hair
•Infertility
•Small pieces of excess skin on the neck or armpits (skin tags)
•Dark or thick skin patches on the back of the neck, in the armpits, and under the breasts
•Missed periods, irregular periods, or very light periods
•Ovaries that are large or have many cysts
•Excess body hair, including the chest, stomach, and back (hirsutism)
•Weight gain, especially around the belly (abdomen)
•Acne or oily skin
•Male-pattern baldness or thinning hair
•Infertility
•Small pieces of excess skin on the neck or armpits (skin tags)
•Dark or thick skin patches on the back of the neck, in the armpits, and under the breasts
Diagnosis of PCOS:
●Ultrasound: This test uses sound waves and a computer to create images of blood vessels, tissues, and organs. This test is used to look at the size of the ovaries and see if they have cysts. The test can also look at the thickness of the lining of the uterus (endometrium).
●Blood tests: These look for high levels of androgens and other hormones. Your health care provider may also check your blood glucose levels. And you may have your cholesterol and triglyceride levels checked.
Treatment of PCOS:
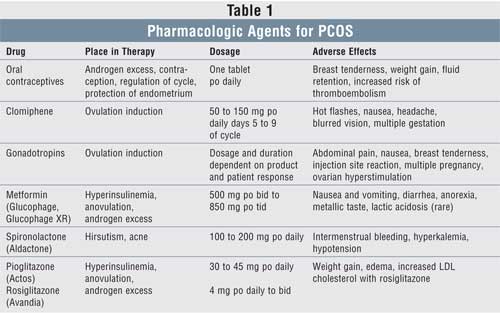
Treatment for PCOS depends on a number of factors. These may include your age, how severe your symptoms are, and your overall health. The type of treatment may also depend on whether you want to become pregnant in the future.
If you do plan to become pregnant, your treatment may include:
A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
Medications to cause ovulation. Medications can help the ovaries to release eggs normally. These medications also have certain risks. They can increase the chance for a multiple birth (twins or more). And they can cause ovarian hyperstimulation. This is when the ovaries release too many hormones. It can cause symptoms such as abdominal bloating and pelvic pain.
If you do not plan to become pregnant, your treatment may include:
Birth control pills. These help to control menstrual cycles, lower androgen levels, and reduce acne.
Diabetes medication. This is often used to lower insulin resistance in PCOS. It may also help reduce androgen levels, slow hair growth, and help you ovulate more regularly.
A change in diet and activity. A healthy diet and more physical activity can help you lose weight and reduce your symptoms. They can also help your body use insulin more efficiently, lower blood glucose levels, and may help you ovulate.
Medications to treat other symptoms. Some medications can help reduce hair growth or acne.



No comments:
Post a Comment
I will reply soon. Thanks for comment.